A Fortune 500 benefits provider embarked on a journey to optimize their claims processing operations, aiming to enhance productivity and deliver exceptional service to their customers. Their challenge? To measure, analyze, and improve the drivers of productivity within this critical department.
The provider set ambitious goals: improve customer and employee satisfaction, streamline claims processing, foster a culture of continuous improvement, and ultimately, achieve significant operational cost savings.
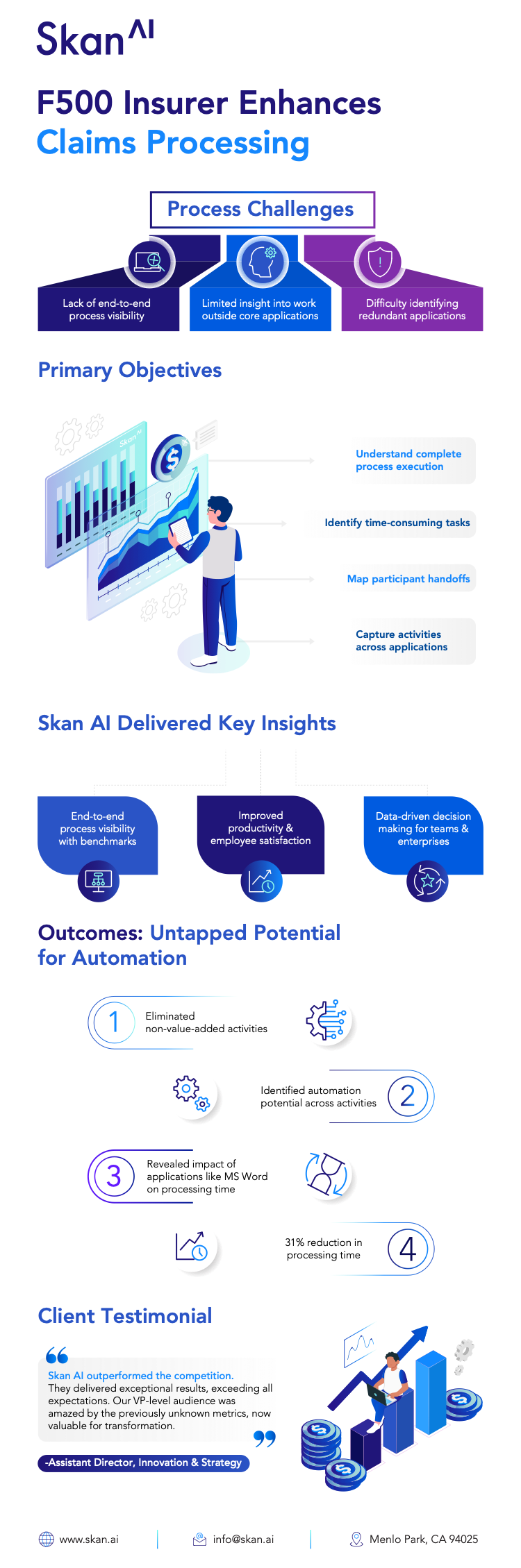
However, they faced several key challenges. They needed to increase workforce utilization and productivity, accelerate workforce proficiency, gain visibility into application usage, and capture capability-based unit cost reductions. Specifically, they lacked visibility into claims process variability, struggled with overstaffing due to low utilization, and faced long claims processing times. Manual tracking of tasks and inefficient processes led to bottlenecks and delays.
Enter Skan AI: Unveiling the Hidden Landscape
To tackle these challenges, they partnered with Skan AI, a platform that provides deep insights into operational processes. The benefits provider initially deployed Skan AI across 200 workstations, focusing on utilization tracking, effort per case, and unit cost. The results were so compelling that they quickly expanded the deployment to 500+ operators.
Skan AI delivered real-time insights into unit cost, processing cost, and required staffing by case type, customer, etc. It also provided claims operations data, quantifying time spent on processing, work time, and non-process work, allowing them to identify and eliminate inefficiencies.
A Transformation Driven by Data
This success story exemplifies how data-driven insights, powered by AI, can transform complex operations like claims processing. By leveraging Skan AI, the benefits provider gained unprecedented visibility into their processes, enabling them to make informed decisions and drive tangible improvements. Their journey demonstrates the power of technology to enhance productivity, improve customer experience, and achieve significant cost savings.
As their VP of Claims Optimization stated, "We log in to our Skan AI Ops dashboard first thing every morning and use it to manage our business in real time throughout each business day. Their insights have transformed how we lead and manage." For any organization seeking to optimize its claims processing operations, this case study serves as a powerful testament to the transformative potential of AI.
The Payoff: Tangible Results
The impact was significant. The provider achieved a customer experience score of 3.5+, exceeded their customer satisfaction target of 50%, and reached a user satisfaction score of 75%. Furthermore, they saw a 65% customer digital adoption rate and, most impressively, realized $4 million in operational expenditure savings five months ahead of schedule. They also improved workforce utilization by 41%, reduced effort per closed case by 16%, and increased decisions/actions per FTE/day by 28%. Furthermore, Skan helped improve capacity forecasting, saving them $1 million in new payroll.
This success story exemplifies the power of Process Intelligence in driving business transformation. By leveraging this innovative approach, a leading insurance provider gained valuable insights into their operations, identified significant cost-saving opportunities, and improved overall efficiency. This data-driven approach empowered them to achieve their strategic goals, and to deliver an enhanced experience to their customers.
Ready to delve deeper? Check out our blog "What Should Insurers Know About Generative AI" for insights on how this cutting-edge technology can further enhance operational efficiency and unlock new possibilities.
Ready to unlock the power of AI in your Insurance operations? Take a look at all we can do for common insurance processes like Claims or Underwriting, and learn how Skan AI’s advanced technology aligns with strategic business priorities to drive significant, scalable improvements across your organization.
